How Using Copper Surfaces Aids Infection Control in Hospital Settings
The antimicrobial power of copper has been harnessed to fight infection for thousands of years. Now more than ever, we should consider its use to mitigate the spread of disease in our healthcare facilities.
“On any given day, about one in 31 hospital patients has at least one healthcare-associated infection,” according to the CDC. In addition to the human-to-human spread, many infections are contracted by touching contaminated surfaces. Surprisingly, in over 30 years of creating antibiotic agents, only three out of 41 are sensitive to most resilient bacteria. The lack of effective agents combined with evidence that less than half of the high touch surfaces in hospitals are clean [1] due to ineffective disinfection processes is cause for concern, and the exceptionally contagious novel coronavirus has only exacerbated the issue. Since studies of coronaviruses have demonstrated that they may survive on surfaces for hours to days depending on temperature and humidity – although surface-to-person transmission is not thought to be the primary mode of infection for this particular coronavirus we might begin to look at using biocidal surfaces as an investment to reduce surface contamination and prevent or treat HAI.
Antimicrobial Materials
A more complete understanding of microbes and their role in disease transmission emerged in the century. The 20th and 21st centuries saw the introduction of antimicrobial finishes as a frontline defense against viruses and bacteria in healthcare settings. While there is an array of new human-made antimicrobial coatings on the market, there are natural antimicrobial materials known to humankind for thousands of years, such as copper and silver alloy.
A meta-analysis of existing literature shows that antimicrobial copper alloys in high touch surfaces reduced the incidence of HAIs by a quarter, increased the probability of recommended Colony-Forming Units (CFUs) threshold by 2.73 times than regular surfaces, and reduced total microbial burden from 37 percent to 100 percent across various studies [2]. A study of ICU rooms in three different hospitals showed that the average microbial burden was 83 percent lower on copper surfaces in those settings [3]. All studies illustrate the antimicrobial and infection prevention capabilities of copper surfaces in clinical environments.
Historically, the antimicrobial outcomes of copper were known by Egyptians in 2600 B.C. mentioned in the papyrus circa (1500 BC) for treating infections, scalds, and itching. [4]. Ancient Greeks also employed copper frequently and this is where the Latin name for copper, cuprous, originated. During the two great European cholera epidemics (1817-1851) copper was ingested for reducing a cholera outbreak after observing smelter workers were unfaceted by the disease [5].
Despite the many benefits of copper, the limited understanding of its antimicrobial process and the discovery of antibiotics reduced interest in its application [6]. Copper has been shown to inhibit growth and destroy microorganisms, including those causing HAIs. The first experiment to show the antibacterial abilities of copper compounds was conducted in 1975 [7]. A series of experiments by Bill Keevil and colleagues in the 1990s demonstrated that different bacteria survived for less time on copper and copper alloy surfaces as compared to stainless steel or plastic. In 2006, experiments showed that antibiotic-resistant bacteria (such as MRSA) was no longer viable on copper within 45 to 90 minutes, whereas bacteria were found to be viable on stainless steel after 72 hours.
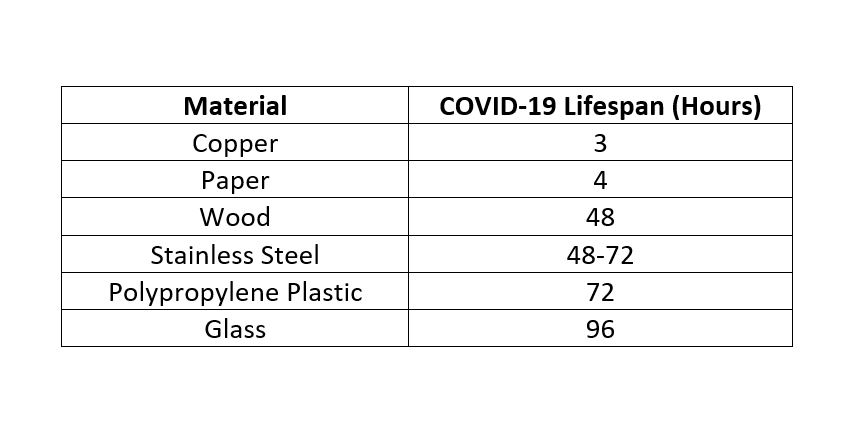
In addition to its antibacterial effects, experiments showed the antiviral properties of copper and copper alloys as early as 1958. Keevil’s team demonstrated the significant reduction of active norovirus after two hours on copper alloys, compared to stainless steel alloys, depending on humidity and temperature. Many recent studies have explored the biocidal effects of copper and copper alloys in hard surfaces. The findings show that the biocidal effects enhance with a higher concentration of copper between 55 percent to 100 percent. Biocidal effects increase by time, with 99.9 percent within two hours of exposure, especially in dry conditions. More recently, Chin and Collogues (2020) explored how long the COVID-virus lasts on common surfaces [8]. They found that the virus lasted the longest on surgical masks and the shortest on copper. Below is a summary of their findings:
COPPER SAFETY & MECHANISM
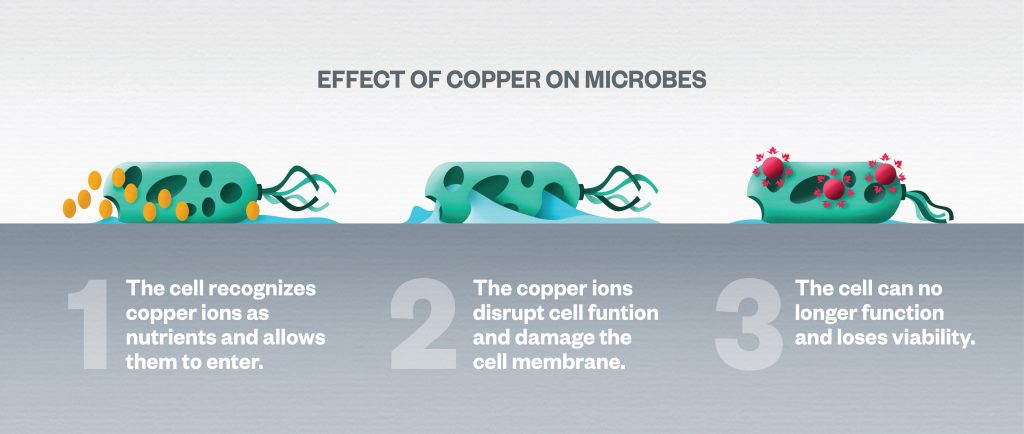
Copper is one of the rare metallic minerals vital for the health of the human body to boost immune response. Although a high concentration of copper is toxic, the external application of copper is safe for humans, and thus it has been used in pipes, dental alloys, or wood preservation, etc. Human cells are capable to metabolize and use cooper. In contrast, microorganisms are very sensitive to higher concentrations of copper and it is thought that copper damages the membrane of the bacterial or viral cell. Other antimicrobial materials such as silver, nickel, or aluminum pose environmental hazards or serious health risks to humans.
HOW DOES COPPER KILL MICROORGANISMS?
Studies suggest that copper interacts with microorganisms on various cellular levels that contribute to cell death by cell membrane permeabilization, membrane lipid peroxidation, protein alteration, and denaturation of nucleic acids. However, long exposure to a low concentration of copper may increase tolerance to copper increasing antibiotic-resistant mechanisms.
The considerable amount of evidence has resulted in the approval of copper alloys as the only hard surface material approved by the U.S. Environmental Protection Agency (EPA), reporting that antimicrobial copper is able to kill more than 99.9 percent of bacteria within two hours of contact as well as inhibiting bacterial growth between cleanings.
While sufficient evidence suggests that the incorporation of copper surfaces reduces the transmission of disease in hospitals, it can, in some cases, be cost-prohibitive. Given the enormous cost of treatment and prolonged length of stay resulting from HAIs and the cost of effective cleaning processes, the initial expense of employing copper materials in hospitals can be regained in a few months. One study showed that applying copper on ten percent of surfaces precludes infections and saves $1,176 per day. A ten-month clinical trial, conducted by Sentara Health in 13 hospitals, found that implementing copper-infused surfaces, overbed tables, and bed rails reduced drug-resistant organisms by 78 percent.
As the quality of evidence from experimental studies indicating the effectiveness of copper application in healthcare environments improves, the fast and broad biocidal characteristic of hard and soft surfaces containing copper may provide a new approach for fighting against HAIs as a complement to standard infection prevention practices. Copper should not replace hand washing, effective PPE use, and other critical infection control practices. The design industry needs additional research to evaluate the efficacy of copper in preventing HAIs and mitigate costs.
The Role of Designers in the Fight Against HAI
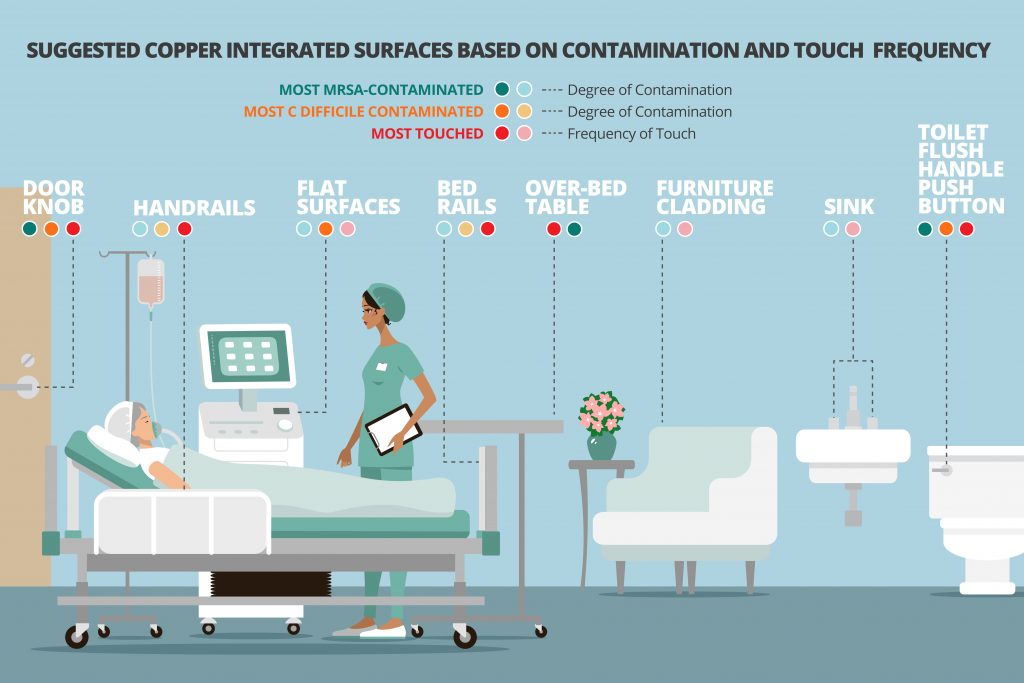
The reality of pandemic consequences will inevitably modify the thought process for both healthcare decision-makers and design professionals that help them retrofit existing or design healthcare facilities of the future. In doing so, design teams can play a vital part in reducing HAIs. As in practicing medicine and healthcare treatment delivery, an evidence-based approach guides healthcare designers in determining which readily available architectural materials and surfaces create opportunities for a more stringent and safer environment. Everything that is touched should be recognized and evaluated since surface contamination plays a vital role in the spreading of HAIs.
Despite the available research, the market is not saturated with copper enhanced materials. The limited product lines of high-touch surfaces available on the market to date include doorknobs, handles, pushbuttons, operating parts, patient bed railings, sinks, plumbing fixtures, copper enhanced solid surface countertops and custom copper layer claddings for furniture.
It is important to note that regardless of type, antimicrobial surfaces natural or human-made can only reduce microbial contamination. It cannot prevent cross-contamination due to poor hand washing or other standard practices. It is a complementary strategy to supplement infection control practices such as thorough cleaning and disinfecting and social distancing where possible.
References
- Carling PC, Parry MF, Bruno-Murtha LA, Dick B. 2010. Improving environmental hygiene in 27 intensive care units to decrease multidrug-resistant bacterial transmission. Crit Care Med 38:1054–1059.
- Pineda, I., Hubbard, R., & Rodríguez, F. (2017). The role of copper surfaces in reducing the incidence of healthcare-associated infections: A systematic review and meta-analysis. Canadian Journal of Infection Control, 32(1).
- Rai S, Hirsch BE, Attaway HH, Nadan R, Fairey S, Hardy J, Miller G, Armellino D, Moran WR, Sharpe P, Estelle A, Michel JH, Michels HT, SchmidtMG.2012.Evaluationoftheantimicrobialpropertiesofcoppersurfaces in an outpatient infectious disease practice. Infect Control Hosp Epidemiol 33:200–201.
- Hodgkinson, V., & Petris, M. J. (2012). Copper homeostasis at the host-pathogen interface. Journal of Biological Chemistry, 287(17), 13549-13555.
- Walusinski O. 2018. The scientific illusion of Victor Burq (1822–1884). Eur Neurol 79:135–149. https://doi.org/10.1159/000487667.
- Arendsen, L. P., Thakar, R., & Sultan, A. H. (2019). The Use of Copper as an Antimicrobial Agent in Health Care, Including Obstetrics and Gynecology. Clinical microbiology reviews, 32(4), e00125-18.
- Majno, G. (1991). The healing hand: man and wound in the ancient world. Harvard University Press.
- Chin, A., Chu, J., Perera, M., Hui, K., Yen, H. L., Chan, M., ... & Poon, L. (2020). Stability of SARS-CoV-2 in different environmental conditions. medRxiv.