Adapting the Emergency Department for Pandemic Readiness and Testing Options with Simulation Modeling
The Emergency Department is the front door of the hospital, serving not only as the first line of response, but also as the first line of defense. So how are architects and researchers reexamining opportunities for expansion, conversion, and separation of spaces within emergency departments to address COVID-19 and future pandemics?
Amid the current COVID-19 pandemic crisis, the need to develop higher levels of readiness has never been more starkly evident. During a highly contagious disease outbreak, the emergency department (ED) is the front door of the hospital, serving not only as the first line of response but also as the first line of defense. Aligning clinical space needs with clinical care needs is of the utmost importance. In the early days of COVID-19, the number of infected and sick patients grew, but questions about transmission modes, infection control needs, and “flattening the curve” were unknowns, which made planning more challenging. However, experience during other mass casualty incidents, in-depth knowledge of healthcare facility needs and requirements, along with predictive analyses such as simulation modeling, can guide rapid response.
Here we share our checklists for evaluating opportunities for expansion, conversion, and separation of spaces in your ED along with our results from a simulation model that uses the SIR (susceptible-infected-recovered) model to predict ED demand. These tools allowed us to quickly develop recommendations to effectively adapt existing ED capacity to meet pandemic screening and care requirements.
Identify Opportunities for Adaptation
Surge capacity under a mass casualty incident is critical to the response effort, but adapting the existing ED to meet that need requires consideration of not only capacity, but care requirements and acuity, infection and transmission risk, and demand. Although hospitals train for different types of mass casualties, many unknowns hamper a cohesive response to a novel virus:
- What is the method of transmission? Are negative pressure rooms necessary or not an issue?
- What is the size of the virus? Will HEPA filtering trap the virus?
- What is the rate of infection and when are people most contagious? Will the onset in the community be sudden or delayed? When will bed capacity become a problem?
- What is the mortality rate? Is the infection a nuisance or a serious community health problem?
The first step in implementing a rapid response ED design is to assess the conditions of the existing department and identify opportunities that can be leveraged quickly with minimal modification. Freeing up capacity through reverse triage and other methods, and adapting existing spaces are critical.
Step 1: Assess existing infrastructure
1. Locate all access points to the facility and identify superfluous entrances and exits.
2. Identify large spaces such as lobbies, auditoriums, and board rooms for conversion to treatment space for low-acuity and non-infectious patients.
3. Categorize the sizes and locations of parking and other outdoor space to situate tents and temporary structures for triage, testing, treatment, and staging of ambulances and EMS vehicles.
4. Ascertain the suitability of adjacent departments (such as observation units, exam rooms, and offices) for segregated treatment of less acute patients, including those with behavioral health conditions.
5. Designate existing circulation elements, such as corridors and elevators, to create a split-flow for transporting patients of varying acuities to other areas of the hospital.
6. Determine the availability of existing Prep/PACU and surgery facilities for emergency treatment.
7. Ascertain the quantity and location of existing negative pressure rooms.
8. Distinguish potential locations for a dedicated space for infected behavioral health patients.
Step 2: Adapt existing spaces
1. Reduce the number of access points. Install a temporary screening station outside each entry to identify high-risk for direct routing to the appropriate care areas. Create separate pods by acuity or infection status using temporary partitions.
2. Utilize prefabricated and modular systems with integrated technology to transform large non-clinical spaces such as auditoriums into ED treatment and support space.
3. Implement external testing facilities in parking areas to reduce the number of walk-in patients.
4. Convert adjacent spaces, such as offices and exam rooms, into treatment for lower acuities.
5. Use color-coded signage to signal new circulation patterns and restricted areas.
6. Utilize existing Prep/PACU and surgery facilities for flexible ICUs as necessary.
7. Group patients with confirmed pandemic conditions into dedicated negative pressure spaces. These spaces can also be designated as high-acuity waiting rooms.
Additional Strategies
1. Transfer non-infectious and less acute patients out of the hospital into alternate care centers.
2. Cohort patients in additional/temporary Airborne Infectious Isolation Rooms (AIIR).
3. Dedicate storage for mobile imaging and other critical equipment within the ED, including dedicated workflow spaces for materials management and patient transport to maximize infection containment.
4. Bring as many services as possible to the patient, particularly imaging and lab.
5. Use ED capacity to transform spaces into critical care units.
Simulation Modeling Rapidly Tests Adaptation Strategies
With the increasing availability of data on transmission and predicted pandemic spread, simulation modeling can predict periods of peak patient flow and optimize equipment, resources, and space. Using data from publicly available information and models, we used facility-focused simulation modeling to determine expected bed and screening needs and to test which capacity adaptations would best meet a patient surge in an ED. We also considered how to best ramp up to the required capacity to screening and access to treatment, while also minimizing the risk of exposure to non-infected ED patients and caregivers.
This case example is based on an ED in the Northeastern US. The ED consists of 99 patient care stations, including beds and recliners in corridors, to accommodate regular overflow. It is divided into five pods, each dedicated to the needs of specific patient types, including pediatric patients, trauma patients, and higher/lower acuity patients. On average, the ED receives 225 patients per day, including 52 ambulance visits. The median patient length of stay was 4.6 hours, based on historical data for the ED.
Modeling Approach
To model expected number of visits and patient needs, we used the SIR epidemic model to predict ED visits and COVID-19 patients based on the number of susceptible people (S) in the specific catchment area of the hospital, estimated infection transmission rates incorporating social distancing (I), and recovery rates (R).
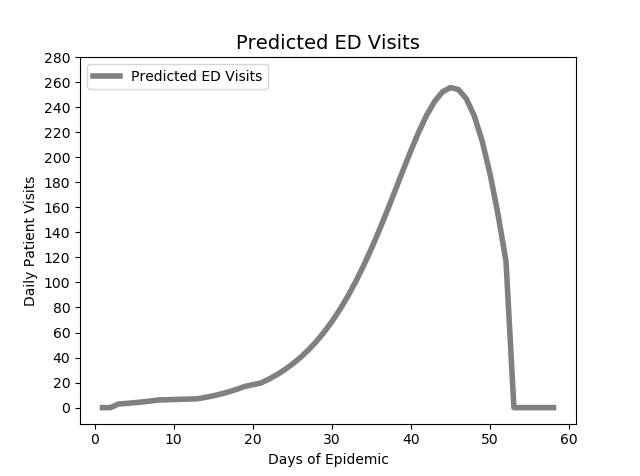
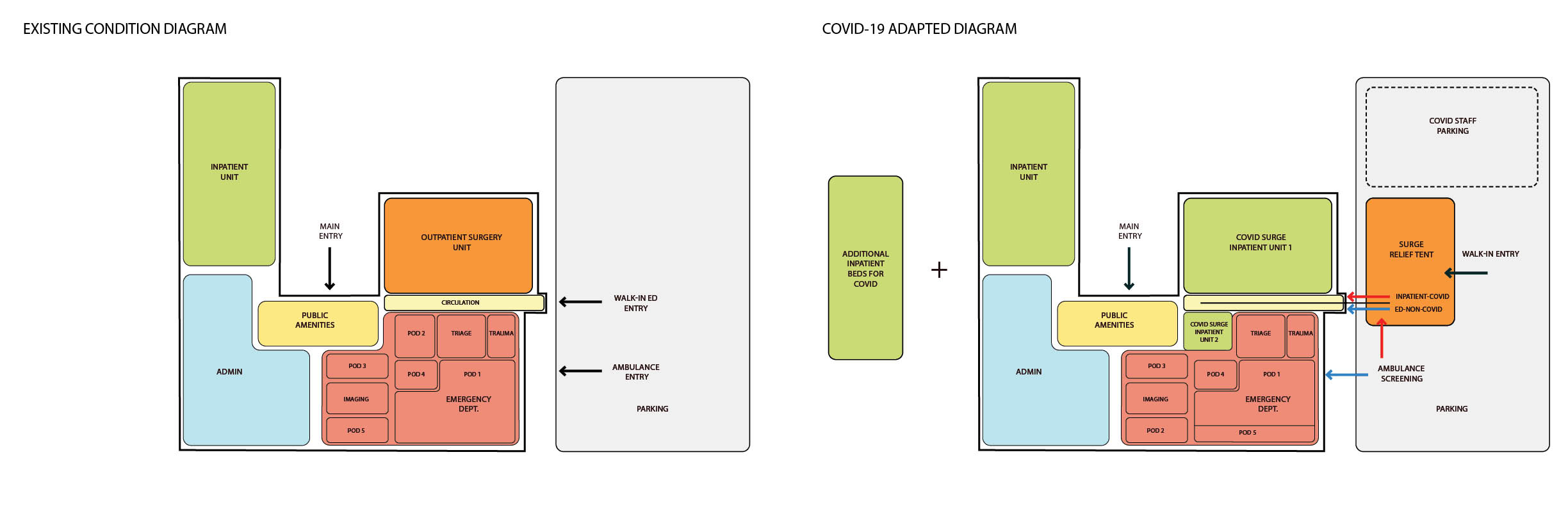
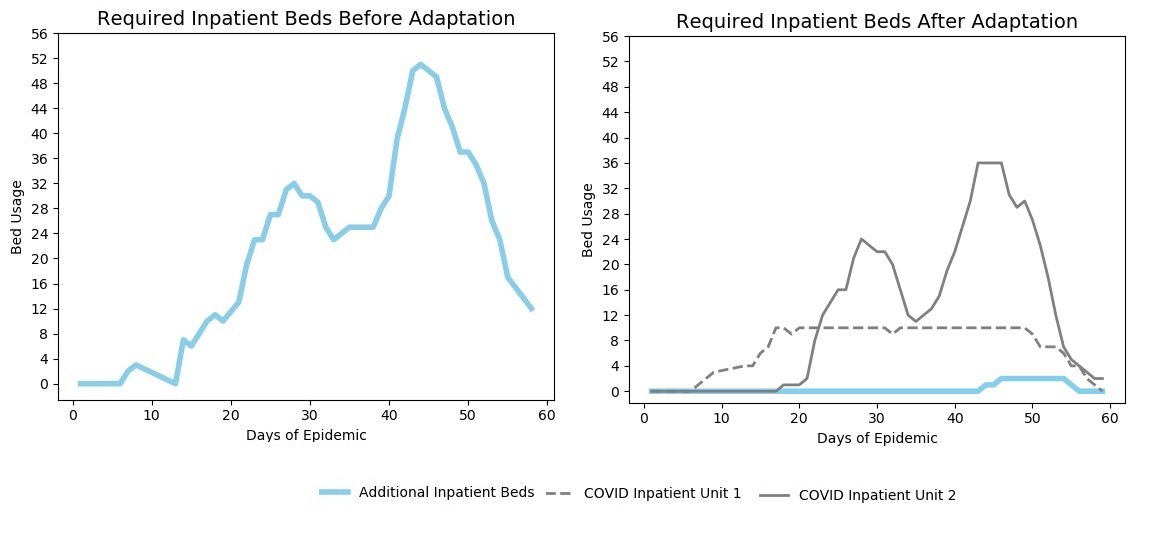
Capacity analysis of the current state revealed that on average days, Pod 1 used 75 percent of available beds at the most. Taking advantage of this potential excess capacity of 25 percent, Adaptation 1 relocated non-COVID patients from Pod 2 to Pod 1, while Pod 2 was converted to COVID-19-only patients. Pod 2 has direct access to the exterior and this reorganization would minimize overlap between COVID-positive and non-COVID patients. Adaptation 2 took advantage of plans already underway to construct a relief tent outside the ED. Adaptation 3 involved transforming the outpatient surgical unit to a COVID-19 inpatient area for up to 34 beds. It has been estimated that approximately 20 percent of COVID patients will be admitted. This change located the two COVID-19 inpatient areas adjacent to each other and maintained distance from regular ED patients. Using our simulation model, we modeled pandemic demand over 60 days and calculated the utilization rates of the ED pods to test whether the adapted layout could meet surge and screening needs.
Results
The results of the simulation demonstrated that these three combined adaptations would accommodate 92% of the inpatient need at the peak epidemic bed demand. While most of the pods would reach higher than generally preferred utilization (greater than 80% occupancy) during some periods, there was some excess capacity available for unexpected events. The two ED-based inpatient COVID-19 units (COVID surge Inpatient Unit 2 (previously Pod2) and the converted outpatient surgery area) would accommodate the needed inpatient beds during the first 20 days of the pandemic without the need for adding inpatient beds elsewhere in the hospital. By absorbing more of the inpatient demand, the adaptation distributed care into unused areas such as the surgery unit.
The optimal configuration for the screening and triage relief tent included four COVID-19 triage rooms, one sorting station, three staff members, and two imaging stations. This configuration would ensure that the maximum waiting time for arriving patients in the tent would be less than 10 minutes.
In this case study, we leveraged an existing simulation model to quickly test adaptations and validate assumptions to implement during a mass casualty incident such as COVID-19. Simulation modeling is increasingly used in the design process but is underutilized to rapidly assess facility adaptation strategies. A refocus on designs that respond to incremental or catastrophic change, promote resiliency to function without significant disruption, and are financially viable – as well as tools to test and adapt them - is needed now more than ever. Our forthcoming blog will outline future-looking design attributes for the change-ready ED.